Case Report: Combination immunosuppression in critical COVID-19 cytokine storm syndrome
Case Report: Combination immunosuppression in critical COVID-19 cytokine storm syndrome
S. Thomas Yadegar, MD and Shahin Delkhah, MD
Providence Cedars-Sinai Tarzana Medical Center
Date of Presentation: March 22, 2020 NEJM360
Case Presentation
A 50-year-old male with no past medical history walked into the emergency department with chief complaints of fever and shortness of breath. He denied any recent travel history or known ill contacts.
Physical Exam
In the emergency department, the patient was noted to have temperature of 37.3C, pulse of 118 bpm, blood pressure of 125/78 mmHg and an oxygen saturation of 91% on room air.
Pertinent Laboratory Values
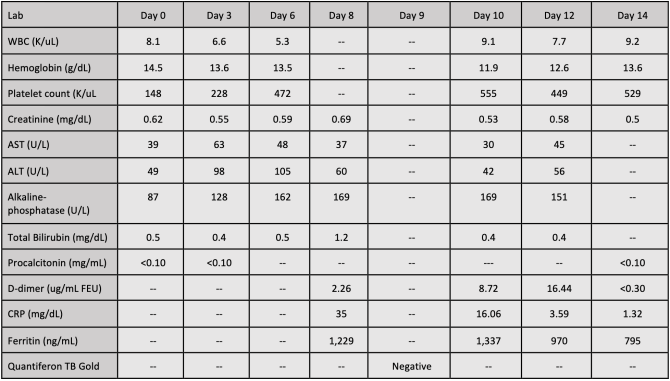
White blood cell count was 8.1 K/uL, hemoglobin was 14.5 g/dL, platelet count was 148 K/uL, and procalcitonin was <0.15 mg/mL. A nasopharyngeal swab testing for SARS-CoV-2 by PCR yielded a positive result three days after initial testing in the emergency department.
Pertinent Imaging
The patient underwent chest x-ray in the emergency department which revealed bilateral diffuse patchy interstitial infiltrates.
Treatment and Outcomes
The patient was admitted to the telemetry floor with droplet and contact isolation. The patient was continued on ceftriaxone 1 g IV and azithromycin 500 mg IV. Four days after admission, the patient was started on hydroxychloroquine (initial dose 400 mg orally twice daily x 1 day; continuing dose 200 mg orally twice daily x 4 days) and azithromycin (initial dose 500 mg once orally; continuing dose 250 mg orally once daily x 4 days). During his hospitalization, patient continued to have fever and shortness of breath and his oxygen requirements varied from 2 LPM to 4 LPM. Six days after admission, the patient developed respiratory distress and progressive hypoxemia. The rapid response team was contacted on the telemetry floor and the patient was intubated and transferred to the intensive care unit. At the time of intubation, he was placed on 100% oxygen. Within 12 hours, the patient’s FiO2 was titrated to 40%. However, the next day, the patient required initiation of IV norepinephrine drip to maintain his blood pressure. As a result of deterioration in clinical status requiring vasopressor support, the patient was given one subcutaneous injection of sarilumab 200 mg eight days after admission. Despite sarilumab injection, the patient developed progressive hypoxemia with FiO2 of 70% that was recorded two days after sarilumab injection. On the third day following sarilumab injection, the patient underwent prone ventilation with 16 hours in the prone position. He was also started on methylprednisolone 20 mg IV every eight hours. The patient continued to require mechanical ventilation. His IV norepinephrine had been decreased, however, his FiO2 concentration remained at 50%. In early April, the patient’s serum CRP improved (Table 1); however, his clinical status did not change significantly. Subsequently, the patient was initiated on mycophenolate mofetil 1000 mg twice daily via nasogastric tube. Approximately 24 hours after initiation of mycophenolate mofetil, the patient’s Positive End-Expiratory Pressure (PEEP) was measured at 14 cm H2O, FiO2 was 40% and prone ventilation had been discontinued. The patient continued on mycophenolate mofetil for two more days, and was de- escalated to methylprednisolone 20 mg IV every 12 hours. Two days after initiation of mycophenolate mofetil, the patient was weaned and subsequently extubated. At the time of this submission, the patient remains in the intensive care unit and has been saturating 99% on 5 LPM.
Lessons Learned
Based on monitoring of ferritin and CRP levels, exclusion of alternate etiologies of patient decompensation and close monitoring of the patient’s clinical status, cytokine storm syndrome was diagnosed and subsequently required combination immunosuppression therapy with sarilumab, mycophenolate mofetil, and systemic glucocorticoids. Critical status COVID-19 cytokine storm syndrome may require combination immunosuppressive therapy to decrease need for prolonged mechanical ventilation, as well as improve the patient’s overall clinical status.