COVID-19 patient with GI symptoms
Dr Steven Fung, Scarborough, Ontario Scarborough Health Network
Case presented at the NEJM360
A 70 year old lady returning to Canada from a trip to South America on March 13. She already develop symptoms of lethargy. PMH is only significant for hypertension and non-insulin dependent diabetes.
Over next 2-3 days, patient began to complain of fever, nausea, diarrhea and anorexia. She finally presented herself to local ER on Mar 16, and was tested for COVID 19. Patient at that time denied any respiratory symptoms, and remain stable with oxygen sat about 97% on room air. She was then discharged home.
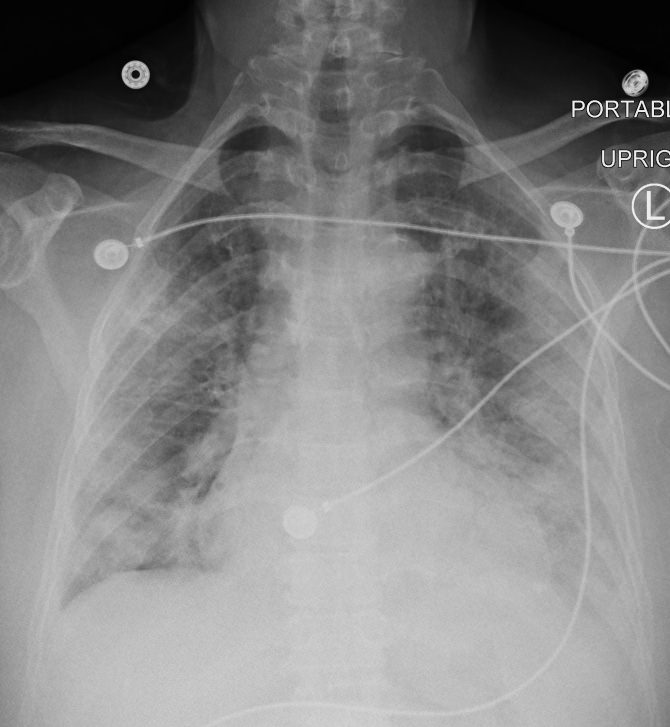
On Mar 17, patient returned back to ER with weakness, and more complaint of more diarrhea. By then, her COVID test returned positive. She had no hypodermic, but was admitted to hospital for dehydration, and intolerance of oral diets as she still complaint of nausea and anorexia. Her CXR on admission was negative.
Over next 2 days, patient gradually became oxygen dependent. She required oxygen 5L on Mar 19, to keep SaO2 >92%. She was seen by ID and respirology, and supportive care was treated with IV Ceftrizxone and Azithromycin. ID recommended against other antiviral therapy.
On March 21, patient’s oxygen saturation dropped further with requirement of 50% FIO2 to keep O2sat >90%. Patient now complaint of SOB, but only occasional cough. Her predominant discomfort was still anorexa, nausea, and diarrhea. Patient was then brought to ICU for optiflow. Patient eventually required intubation on March 22.
Lesson: Patient with COVID 19 can present with predominantly GI symptoms with no respiratory complaint. It has been reported on literature that COVID 19 patients with predominant GI symptoms have poor prognosis